The Crucible of Covid
Famed researcher David Ho, MD (BS ’74), on what we learned about science and society during the pandemic — and how those lessons could help prevent the next one.
by Dale Keiger
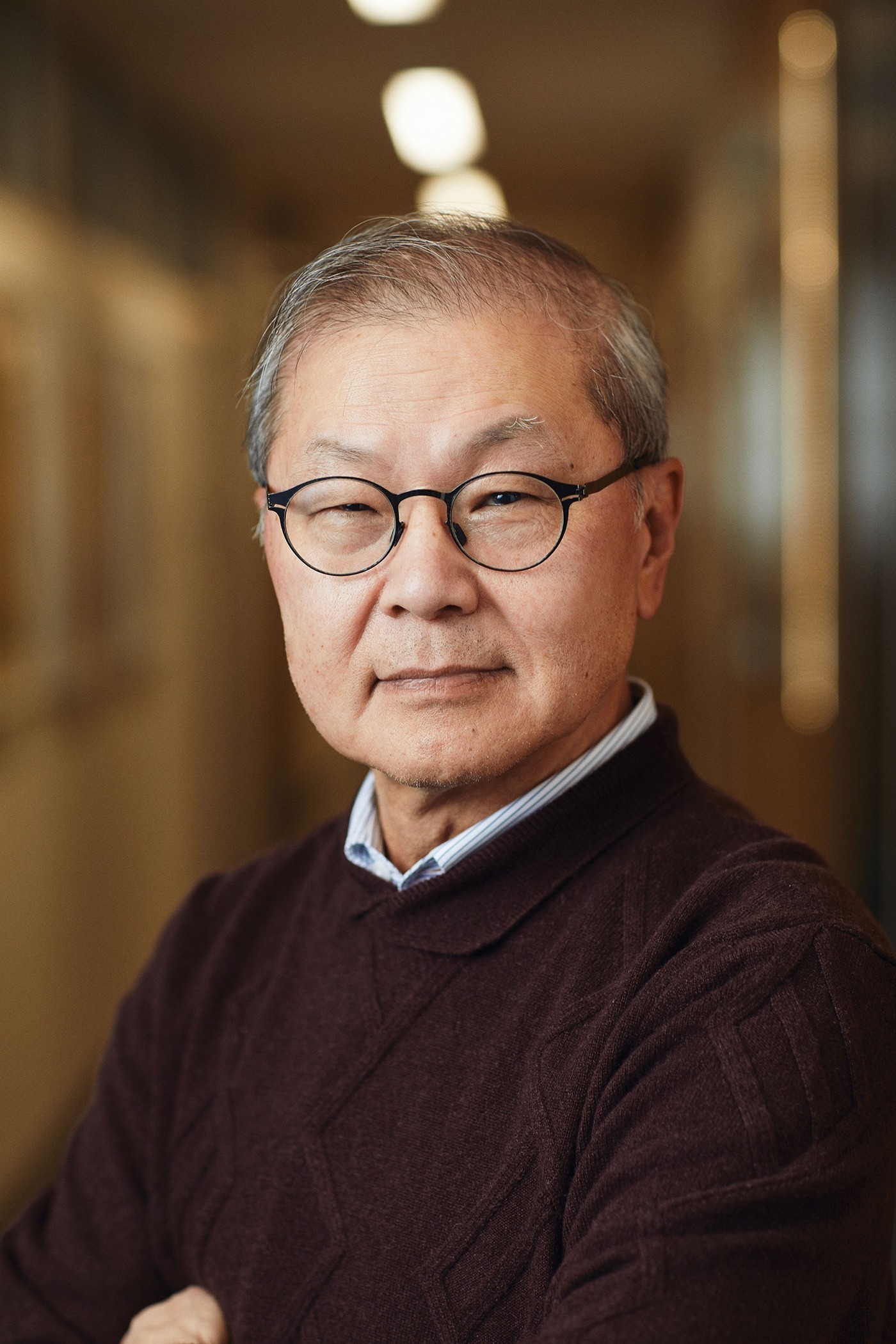
Photography by Stephanie Diani
The global challenge of the COVID-19 pandemic mobilized countless scientists around the world to understand the coronavirus and develop tests, vaccines, treatment, and prevention protocols. Prominent among them is virologist DAVID D. HO, MD (BS ’74), director of the Aaron Diamond AIDS Research Center at Columbia University. Famous for pioneering combination antiretroviral therapy for HIV-positive patients in the 1990s, Ho is now working on treatments and vaccines for the SARS-CoV-2 coronavirus responsible for COVID-19 and is part of an international effort to discover and engineer antibodies that can neutralize the virus. He recently took the time to discuss the long-term lessons of the pandemic with Techer.
“We’re going to have even better drugs, antibodies, and vaccines to come, and some of them could be even broader in their protective effect and extend beyond just the COVID-19 virus and cover other related viruses. That gives me hope that better tools are going to come along.”
We are more than two years on from the Wuhan outbreak. Did the COVID-19 pandemic play out as you anticipated?
On the academic side, it’s probably bigger than any of us had imagined, with wave after wave and, of course, over a quarter-billion people infected and five million dead. I think the other thing is [that] we knew there was enormous scientific investment in solving this problem, but the solutions came faster than we anticipated, exemplified by the very rapid development of highly efficacious vaccines and antibody therapies and more recently, the emergence of treatment drugs. I think that’s beginning to change the equation. We now have more tools at our disposal to combat this virus.
The global health system did a pretty good job of containing SARS and MERS. What was so different about COVID-19?
Both MERS and SARs were actually more deadly. But there’s one very fundamental difference with COVID-19, and that is people who are infected can have no symptoms at first and so go about their business and spread the virus. That’s a particular feature that allows it to spread so rampantly.
In August 2020, on a podcast, you said the country was doing very poorly confronting the pandemic. More than a year from that statement, what’s your assessment? Did we get better?
I think we did get better but we could always improve. Witness the period following the summer of 2020—the situation got a lot better until the winter months arrived. That’s because I think much of the country was hit hard and was devastated and everybody learned the lesson the hard way. Then the winter months and the holidays and the increased indoor contact caused another peak. Once the situation was better, everyone let their guard down. Now, you could say nearly two- thirds the country is vaccinated, so the pool of susceptible individuals has decreased substantially, so the expectation was that we may not hit the same type of peaks that we have seen in the past. But the omicron variant has proven that wrong because its infectiousness is several fold greater than previous variants. I think we need to sustain our efforts much longer than what we have done with each previous wave of the pandemic.
What made such a difference this time in the extraordinarily rapid development of multiple vaccines and now-promising treatments?
After China shut down in January 2020 and we pretty much shut down here in March, everyone appreciated the enormity of the situation. There was a massive infusion of talent to address this problem from a diagnostic, treatment, and prevention perspective. And the FDA should get credit for responding very quickly to fast-track the development of antibody drugs and vaccines.
But these developments don’t come out of nowhere. There was a lot of scientific progress made on various vaccine platforms, most notably the mRNA vaccines administered by Pfizer and Moderna. Some of that technology had been worked on for over a decade. In terms of antibodies and drugs, the massive effort spent on HIV and hepatitis C really formed the foundation for rapid development. Take the Pfizer drug: It is a protease inhibitor that was first developed in the 1990s for HIV and then applied to hepatitis C and now effectively applied to COVID-19.
Does this give you some hope going forward? This is not going to be our last pandemic.
That’s absolutely right. Some of these drugs are likely to hit related coronaviruses that have been found in animal species, particularly in bats. Some of the antibodies that scientists are coming up with will also hit related viruses. Just as one example: We have developed an antibody that will hit not only COVID-19 but SARS and all the related viruses that we have examined that are normally found in bats. We are already developing useful interventions that might block a subsequent emergence of a related coronavirus.
We’re going to have even better drugs, antibodies, and vaccines to come, and some of them could be even broader in their protective effect and extend beyond just the COVID-19 virus and cover other related viruses. That gives me hope that better tools are going to come along.
Some of the more optimistic thinking has been that we will approach a point with COVID-19 where it just becomes part of our public health landscape, like influenza. When might we reach that point?
I’ve been espousing such a point of view, but I don’t know when we might get there. The omicron variant being more infectious yet less pathogenic may, oddly enough, rip through the population and raise herd immunity in a way that helps to end the pandemic and turn it into an endemic situation. I’m hoping that 2022 is the last year we have to deal with the severe devastation caused by the virus. I think with multiple effect drugs and antibodies available now, and, in this country, three vaccines available, we should be able to eliminate the severe consequences of COVID-19 and turn it into something that is not as fearsome and more manageable, more treatable
What are the most significant things that we have learned from this experience?
I think it’s pretty clear that these types of pandemic threats are as important as climate change. I think that’s been the case for a long time but it’s never been fully appreciated until this pandemic hit us. This is the third coronavirus in the last 20 years. Surely there’s going to be more, because we know these viruses are prevalent in various animal populations and we’re going to have more cross-species transmission from animals to humans. If we don’t do a good job at the outset of each transmission to contain it, we’re going to endure yet another epidemic and possibly a pandemic. I worry that even if we successfully control this COVID-19 pandemic, we will very quickly forget the lessons and become once again complacent. This is a major security threat, not just to our country but to the world.
I also fear for our inability to sort out facts. Science has given us the vaccines and drugs that allow us to begin to rein in this pandemic, but if people believe in their own set of facts and that these things don’t work, then all the work would be for naught. That would be a huge tragedy. I think scientists need to continue to help put out the truth and explain the facts in ways that are much more understandable to a layperson. We need to wipe out the spread of misinformation in the same way we do for the spread of pathogens.

Dale Keiger retired as editor of Johns Hopkins Magazine in 2018. From a house in the woods outside Baltimore, Maryland, he continues to scribble, mostly about science, music, and the deep weirdness of existence. He is also a photographer and a walker.He collected
35 years of profiles in the anthology The Man WhoSigned the City, (10,000 Days Press,2019), available from fine Amazons everywhere.